Week 2 - Introduction to Medical Models
Session 3 - Comparing and contrasting the Biomedical and Biopsychosocial models of health
- Summary Reflections and Lecture Questions
- Activity 1.2.3.1: The Case of Mrs Chatsworth
- Learning Outcomes: Comparing and contrasting the Biomedical and Biopsychosocial models of health.
Summary Reflections and Lecture Questions
1) Which statement is most correct with regard to the epistemological foundations of the biomedical model?
a) The biomedical model basis its claims to knowledge on interpretivist thought – the idea that observations and hypotheses need to be interpreted by qualified individuals.
b) The biomedical model basis its claims to knowledge on positivist thought – the idea that observations and hypotheses need to be scientifically verified.
c) The biomedical model is holistic in its consideration of how the body functions.
d) The biomedical model is reductionist in its consideration of how the body functions
2) Which statement is most correct with regard to the assumptions underlying the paradigmatic approach of the biomedical model?
a) The patient is seen as an active participant in their own health.
b) Biomedicines traces the cause of diseases to multiple factors.
c) The focus of biomedical care is on keeping people healthy.
d) Biomedicine is invested in technologies which help it to make sense of biological aspects of disease.
Bio-Psycho-Social is the holistic approach to health, disease, and illness
The biopsychosocial model of health takes a more comprehensive approach by considering:
- Various aspects of health beyond just the physical body.
- The impact of behaviours on health choices and help-seeking behaviour.
- The promotion and maintenance of health through social, environmental, and behavioural changes.
- Social solutions as part of addressing health issues within society.
The Biopsychosocial model integrates its holistic approach with the Biomedical Model. According to George Engels (1977), to fully understand the factors that contribute to disease and to provide effective healthcare, a medical model should consider:
- The patient as an individual
- The social context in which the patient lives
- The doctor’s role in the patient’s care
- The broader healthcare system
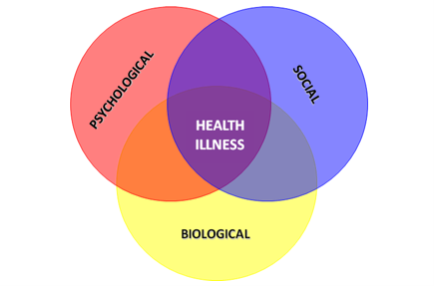
Aspects of the Biopsychosocial Model
Explanatory Aspect:
- Composite model: Behavior and disease are shaped by the interactions of biological, psychological, and social factors.
Treatment Aspect:
- Multidimensional approach: Illness and disease are treated with a comprehensive plan that at the same time addresses medical, psychological, family, and social factors.
- “Bio”: Biological => Clinical aspects.
- “Psycho”: Psychological => Individual/personal factors.
- “Social”: Social => Contextual, environmental, and occupational factors.
The Biopsychosocial model has multiple layers
- Microscopic (gene/molecule/cell):
- Genetic makeup
- Biochemical pathways
- Organ/organ system:
- Physiology
- Homeostasis
- Individual:
- Identity
- Sick role
- Attitudes and lifestyle
- Family:
- Support
- Expectations
- Housing
- Life opportunities (or lack thereof)
- Community:
- Accessibility of health and social services
- Resources for self-care and rehabilitation
- Opportunities for unhealthy lifestyle choices (e.g., drugs)
- Environment:
- Economic and political influences
Each layer influences and interacts with the others, emphasizing that health is not just the result of biological factors but is also shaped by psychological and social dimensions.
The aim of the Biopsychosocial (BPS) Model is to promote overall wellness by addressing multiple dimensions of well-being. The model recognizes that true wellness is achieved through the balance and integration of the following aspects:
- Emotional wellness : Coping effectively with life and creating satisfying relationships.
- Financial wellness: Satisfaction with current and future financial situations.
- Social wellness: Developing a sense of connection, belonging, and a well-developed support system.
- Spiritual wellness: Expanding our sense of purpose and meaning in life.
- Occupational wellness: Personal satisfaction and enrichment derived from one’s work.
- Physical wellness: Recognizing the need for physical activity, diet, sleep, and nutrition.
- Intellectual wellness: Recognizing creative abilities and finding ways to expand knowledge and skills.
- Environmental wellness: Good health by occupying pleasant, stimulating environments that support well-being.
The model emphasizes that wellness is a multidimensional and dynamic state that is achieved through a holistic approach to health, integrating these various aspects of life.
Some limitations of the Biopsychosocial (BPS) model:
- Healthism: The BPS model may promote an excessive focus on personal health and lifestyle modifications as the primary means to achieve well-being. This can lead to moral judgments about health behaviours and increased pressure on individuals to fit into societal norms of a “healthy lifestyle.”
- Laymanisation: While the BPS model encourages holistic health practices, it may also contribute to the trend of non-professionals taking on roles traditionally held by healthcare providers. This can lead to the potential for misinformation or inadequate care if individuals lack the necessary expertise.
- Medicalisation: The BPS model’s broad perspective can sometimes lead to the medicalisation of normal human experiences, where non-medical issues are framed as health problems. This can result in unnecessary interventions and a pathologization of everyday life.
- Pharmaceuticalisation: With the BPS model’s inclusion of biological factors, there is a risk of over-reliance on pharmaceutical treatments. This can overshadow other aspects of health, such as social and psychological factors, and promote a narrow, medication-centric approach to well-being.
Activity 1.2.3.1: The Case of Mrs Chatsworth
1. From the perspective of the biomedical model, what might you say are some of the factors that affect Mrs Chatsworth’s recovery?
- Post-operative complications: Chronic inflammation in her knee and thigh region following the hip arthroplasty
- Muscle atrophy: Reduced muscle mass and definition in her quadriceps and gluteal muscle groups, leading to decreased balance and mobility.
- Osteoarthritis: Chronic osteoarthritis in her knees, hips, and shoulders, which affects her overall joint function and mobility.
- Partial weight-bearing status: Limited weight-bearing capacity due to pain and stiffness in her right hip.
- Chronic pain: Persistent pain due to both osteoarthritis and the recent surgery.
2. What could the treatment plan for Mrs Chatsworth be from a biomedical perspective?
A treatment plan from a biomedical perspective would likely focus on:
- Pharmacological management: Adjusting her pain medication to better control post-operative pain and inflammation, possibly introducing anti-inflammatory medications.
- Physical therapy: A structured rehabilitation program targeting muscle strengthening, especially in the quads and glutes, to improve her mobility and balance.
- Orthopaedic evaluation: Ongoing assessment by an orthopaedic surgeon to monitor the healing of the hip replacement and manage any complications.
- Assistive devices: Continued use of elbow crutches or a walker to aid in mobility while she regains strength. Could also use a wheelchair
- Pain management interventions: Possible consideration of injections, drips, or other interventions to manage chronic osteoarthritis pain.
3. From the perspective of the biopsychosocial model, what might you say are some of the factors that affect Mrs Chatsworth’s recovery?
From a biopsychosocial perspective, factors affecting her recovery include:
- Psychological factors: Grief and emotional stress following the recent loss of her husband, which may contribute to a sense of isolation and decreased motivation to engage in her recovery.
- Social factors: Limited social interaction and support outside of her daughter and grandchildren, potentially leading to loneliness and decreased well-being.
- Environmental factors: Living in an apartment without a lift, making daily activities such as climbing stairs more difficult.
- Physical health factors: Chronic conditions such as osteoarthritis and hypertension, complicating her physical recovery.
- Economic factors: Financial stress due to medical expenses not fully covered by insurance, leading to anxiety about future healthcare costs.
4. What could the treatment plan for Mrs Chatsworth be from a biopsychosocial perspective?
A biopsychosocial treatment plan would be more holistic and might include:
- Psychological support: Grief counseling or therapy to address her emotional well-being and help her cope with the loss of her husband.
- Social support: Encouragement to engage in community activities or social groups, particularly those aligned with her interests, like her religious community, to reduce isolation. Join a support group where people suffer from similar health issues limiting her Isolation and loneliness.
- Home modifications: Assessing her living environment and possibly relocating to a more accessible home, or installing aids to make her current apartment safer and easier to navigate.
- Chronic disease management: Regular follow-ups with a primary care physician to manage her osteoarthritis and hypertension.
- Financial counselling: Assistance with managing her finances, potentially exploring options for financial support or more cost effective healthcare solutions.
- Physical therapy: A rehabilitation program incorporating a more flexible, patient-centred approach that accounts for her psychological and social circumstances.
5. What would be the limitations of each of these models be when coming up with a treatment plan for Mrs Chatsworth?
Biomedical Model Limitations:
- o Focuses on physical symptoms and medical treatment, potentially overlooking important psychological and social factors that affect her overall well-being and recovery.
- o May lead to over-reliance on medication and surgery without addressing underlying emotional or social issues.
Biopsychosocial Model Limitations:
- Can be complex and resource-intensive, requiring coordination across multiple disciplines, which might not be feasible for all patients.
- May be less effective in addressing acute medical conditions or when a specific biomedical intervention is urgently needed.
- Psychological and social interventions may take time to show effects, potentially delaying immediate physical recovery.
Learning Outcomes: Comparing and contrasting the Biomedical and Biopsychosocial models of health.
Define ontology and epistemology.
- Epistemology
- The way we know things.
- Descriptive in nature.
- Ontology
- The way thing really are.
- Binary in nature.
Describe the biopsychosocial model and discuss how it acts as an alternative to the biomedical model.
- The biopsychosocial model of health takes a more comprehensive approach by considering:
- Various aspects of health beyond just the physical body.
- The impact of behaviours on health choices and help-seeking behaviour.
- The promotion and maintenance of health through social, environmental, and behavioural changes.
- Social solutions as part of addressing health issues within society.
Compare and contrast the biomedical model with the biopsychosocial model of health.
- Biomedical model
- Onto-epistemological assertion
- Framework
- a set of philosophical commitments
- An approach to conceptualise disease
- Disease is presumed to be fully attributed to physiological or biochemical deviations from the norm
- Suggests disease is detected and identified through a process of observation, descriptions, and differentiation
- Biopsychosocial model
- Explanatory Aspect:
- Composite model: Behavior and disease are shaped by the interactions of biological, psychological, and social factors.
- Treatment Aspect:
- Multidimensional approach: Illness and disease are treated with a comprehensive plan that at the same time addresses medical, psychological, family, and social factors.
- “Bio”: Biological => Clinical aspects.
- “Psycho”: Psychological => Individual/personal factors.
- “Social”: Social => Contextual, environmental, and occupational factors.
- Multidimensional approach: Illness and disease are treated with a comprehensive plan that at the same time addresses medical, psychological, family, and social factors.